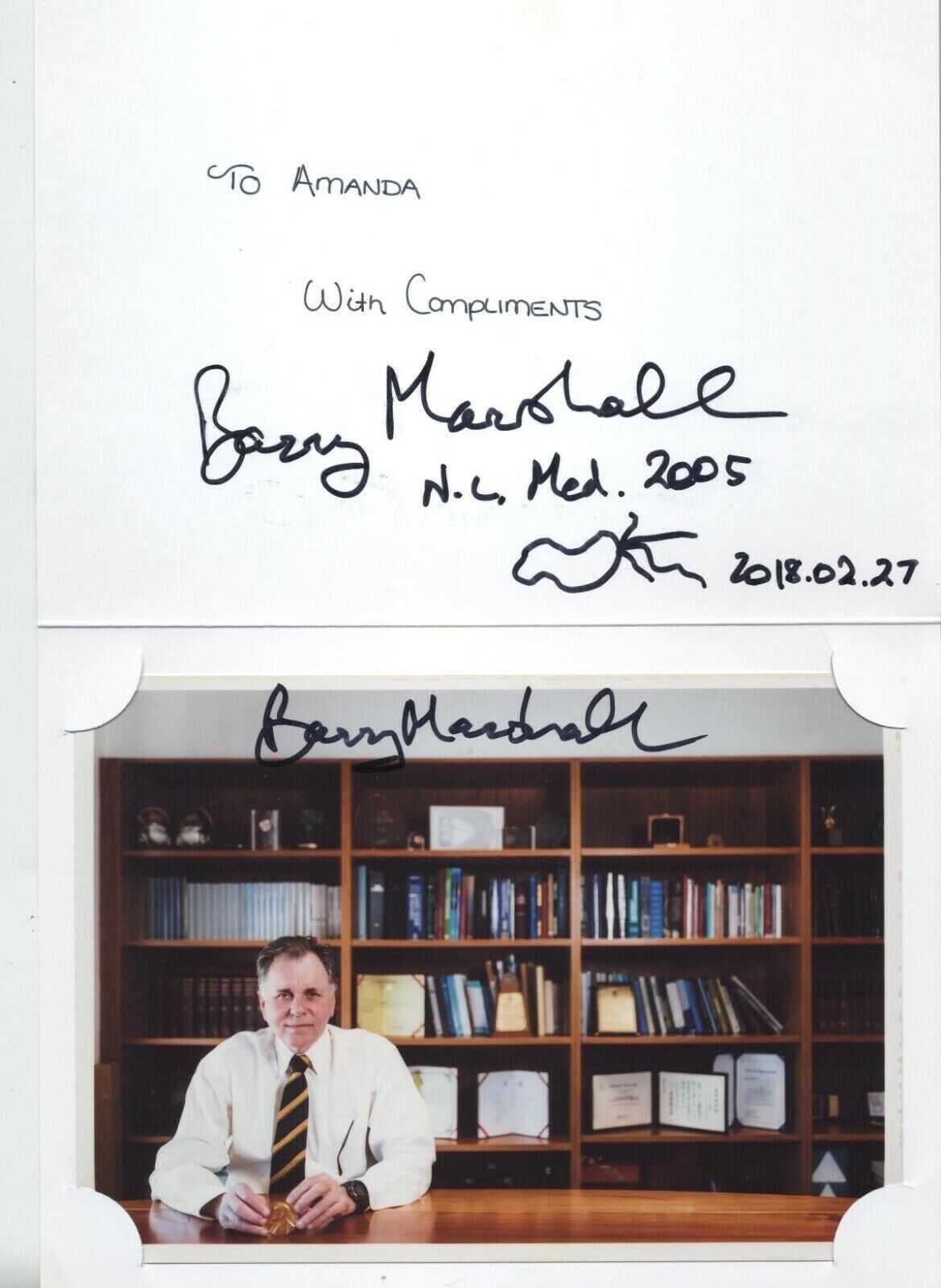
NOBEL PRIZE MICROBIOLOGY SKETCH BARRY MARSHALL AUSTRALIA ULCERS BACTERIA For Sale
When you click on links to various merchants on this site and make a purchase, this can result in this site earning a commission. Affiliate programs and affiliations include, but are not limited to, the eBay Partner Network.
NOBEL PRIZE MICROBIOLOGY SKETCH BARRY MARSHALL AUSTRALIA ULCERS BACTERIA:
$250.48
AN AUTOGRAPH FROM 2018 ON THE UNIVERSITY OF WESTERN AUSTRALIA THE MARSHALL CENTRE FOLDER WITH ORICIAL SIGNED PHOTO SIGNED AND A SKETCH WITH SIGNATURE VOF A BACTERIUM.Marshall, (born September 30, 1951, Kalgoorlie, Western Australia, Australia), Australian physician who won, with J. Robin Warren, the 2005 Nobel Prize for Physiology or Medicine for their discovery that stomach ulcers are an infectious disease caused by bacteria.October 4, 2005 -- The University of Virginia is celebrating the announcement that Barry Marshall, M.D., professor of Research in the School of Medicine, was awarded the 2005 Nobel Prize in physiology or medicine. Marshall is the first current member of the University of Virginia School of Medicine faculty to be honored with a Nobel Prize.
“We congratulate Dr. Marshall for winning the Nobel Prize in medicine,” said Arthur Garson, Jr., M.D., Vice President and Dean of the School of Medicine. “His work highlights the spirit of innovative and critical thinking that the UVa School of Medicine fosters.”
Marshall and pathologist Robin Warren, M.D., discovered the connection between Helicobacter pylori bacterium and peptic ulcers and gastric cancers in Australia in the early 1980s.
Marshall then spent a decade (1986-1996) at the University of Virginia as a research fellow, gastroenterologist and professor of medicine.
“It is a great thrill to be recognized in this way and it is fitting that a lot of the credit for the dissemination of the new discovery goes to faculty at UVa,” Marshall said. “In Charlottesville I was able to develop important diagnostic tests which were needed in order to implement the new discoveries.”
Since he returned to Australia, Marshall has remained on the UVa School of Medicine’s faculty as a professor of research and internal medicine.
“While he was at U.Va., (Dr.) Marshall worked to strengthen the evidence that H. Pylori is the cause of peptic ulcers and gastric cancer, and other health conditions,” said Dr. Robert Carey, David A. Harrison III Distinguished Professor of Medicine and University Professor at UVa. Dr. Carey was dean at the UVa School of Medicine during Marshall’s tenure. “He had only a theory when he came here, but when he left, his findings were well accepted.”
Carey said Marshall told him in a recent conversation that he would accept the Nobel Prize on behalf of the University of Virginia and the University of Western Australia.
Marshall’s research was revolutionary, in that it changed the understanding of ulcers and gastrointestinal diseases, according to Dr. David Peura, UVa Professor of Medicine and President of the American Gastroenterological Association.
“His work was unprecedented, especially since he was a clinician and not a researcher,” Peura said. “I was treating my patients with the then traditional methods for ulcers when his work was first published and I truly did not believe it until I saw what it did for my patients.”
Peura joined the UVa School of Medicine faculty in 1990, because of his desire to work with Marshall.
“His perseverance was astounding. Most people would have abandoned their work in the face of the opposition and dismissal that he originally received,” Peura said.
The Nobel Prize for medicine is awarded by the Karolinska institute in Stockholm as stated in the will of Alfred Nobel, a Swedish industrialist who founded the prestigious awards in 1895.Barry J. MarshallThe Nobel Prize in Physiology or Medicine 2005
Born: 30 September 1951, Kalgoorlie, Australia
Affiliation at the time of the award: NHMRC Helicobacter pylori Research Laboratory, QEII Medical Centre, Nedlands, Australia, University of Western Australia, Perth, Australia
Prize motivation: "for their discovery of the bacterium Helicobacter pylori and its role in gastritis and peptic ulcer disease."
Prize share: 1/2
LifeBarry Marshall was born in Kalgoorlie, Australia, but spent his childhood from the age of eight in Perth, where he also studied to become a doctor. It was during his employment at the Royal Perth Hospital that he carried out the work with colleague Robin Warren that led to his receiving the Nobel Prize. Barry Marshall has continued his affiliation with the hospital and university in Perth, but is also connected to US universities, including the University of Virginia in Charlottesville. He is married with four children.
WorkGastric ulcers are a common illness, but their cause was long unknown. It was discovered that the most common cause is bacterial infection. After Robin Warren discovered colonies of bacteria at gastric ulcer sites, he was contacted by his colleague Barry Marshall, who then successfully cultivated the previously unknown bacteria Helicobacter pylori. Robin Warren and Barry Marshall proved in 1982 that patients could only be cured if the bacteria were eliminated. This is now achieved by treatment with antibiotics, and gastric ulcers are no longer a chronic illness.
To cite this sectionMLA style: Barry J. Marshall – Facts. NobelPrize.org. Nobel Prize Outreach AB 2021. Sun. 15 Aug 2021. to topLearn moreNobel Prizes 2020Twelve laureates were awarded a Nobel Prize in 2020, for achievements that have conferred the greatest benefit to humankind.
Their work and discoveries range from the formation of black holes and genetic scissors to efforts to combat hunger and develop new sale formats.
See them all presented here.Nobel Prizes 2020 graphicsExplore prizes and laureatesLook for popular awards and laureates in different fields, and discover the history of the Nobel Prize.Select the category or categories you would like to filter SciencesDecrease the year by one-Choose a year you would like to search in2005Increase the year by one+ExploreThe Nobel Prize in Physiology or Medicine 2005Barry J. MarshallJ. Robin WarrenShare thisFacebookTwitterLinkedInEmail this pageBarry J. MarshallBiographicalIwas born in 1951 in Kalgoorlie, a prosperous mining town 370 miles east of Perth, Western Australia. Kalgoorlie was a gold rush town which sprang up in the desert after the Irishman Paddy Hannan struck gold there in 1892.
At the time I was born my father was 19 years old and in the final year of his apprenticeship as a fitter and turner. My mother quit her nursing training to have me at the age of eighteen years.
We moved quite a bit through my early childhood. After my father finished his apprenticeship, my parents decided to go and work in the new Uranium mine in Rum Jungle in the Northern Territory. They drove their Model A Ford up Australia’s west coast about 1000 miles but stopped at Carnarvon when the car broke down. The whaling station at Carnarvon was also offering excellent wages for good tradesmen and my father was one of the best. We lived near the whaling station while I grew from two to four years and my brother William was born there.
My first memories are of life in Carnarvon. I recall a boat trip back to Perth on one occasion and a DC3 aeroplane flight to Perth on another. Our house was on Babbage Island about 100 yards from the beach. We had electricity, an outhouse toilet, dirt floors in parts of the house, a telephone, refrigerator, a car, a cat and a dog. Nearby was a derelictsteam engine on a railway siding. We had neighbours close by and other kids to play with.
By then, my grandparents had the license on the Tower Hotel in Kalgoorlie and periodically we would return there to live. In Kalgoorlie I remember doing all kinds of things as a six and seven year old including making bows and arrows, slingshots and lighting crackers after school.
After a period back in Kalgoorlie, my mother decided to move the family to Perth where my second brother, Andrew, was born in 1958. I was seven years old at the time. I suppose my mother could see the young boys in Kalgoorlie leaving school at 16 and going down the mines to work. It was an attractive proposition for them. They earned high salaries and had a wild social life drinking and partying on their off days. She wanted more for her children and hoped we would study and enter a profession. Moving to the city was the first step. We are lucky she made that decision. My two brothers and sister all went through University and have highly successful careers and happy lives.
In school I sporadically hit the top of the class but mostly did not work hard enough to stay up there. At home I had plenty of interesting reading material. Dad always explained the car engine when he repaired it and he had many technical books so I was making electromagnets by age eight as well as reading my mother’s medical and nursing books. I suspect I was born with a boundless curiosity and this was encouraged through my childhood.
Being the eldest of four children, I was expected to be the responsible one and often found myself controlling two younger brothers who shared my exuberant and inquisitive nature. I still feel guilty about the time I advised my younger brother to jump out of a tree and he broke his arm.
My first exposure to fame came at age twelve when I was left in charge of the younger siblings while my mother attended to the grocery shopping. I had a history of responsible baby-sitting by this time so nothing should have gone wrong. During the morning my 18 month-old sister found a milk bottle half full of kerosene and drank some, perhaps also aspirating a little so that my brothers and I found her choking but did not know why. I called the emergency services and an ambulance arrived about fifteen minutes later. During the wait, as I had learned some basic CPR at the Royal Lifesaving Society Swimming training, I tried to perform mouth to mouth resuscitation on my little sister. I know now that it was pointless because she was actually still breathing. However, my close mouth contact enabled me to smell the kerosene and make the diagnosis of poisoning. I featured in the newspaper a few days later, with my fully recovered little sister on my lap. It was a good story about how to call the emergency number, and why you should not put poison into drink containers. Very kindly my mother did not leak to the press the fact that it was I who had left the kerosene within reach of young Marie!
In our dad’s shed, my brothers and I had access to all the tools needed to build or dismantle anything. I frequently got into trouble doing both. My favourite book as a child was an old Newne’s Children’s Encyclopaedia which my grandfather had bought just before World War II and donated to our family after seeing how interested we were in it. Each volume had special chapters called “Things Boys can Do”. My brothers and I would pick out interesting projects. As the years went by, and I grew up, I recall building a slingshot, a crystal set, a Morse-code set, various guns, a hydrogen generator for balloons, electric devices and minor explosives. In those days fireworks had been banned, but chemicals were easily available from pharmacies and chemical suppliers so, in the tradition of Alfred Nobel, we would create various explosive mixtures and make firecrackers and bombs. This started rather benignly with simple gunpowder but graduated to more dangerous oxidising agents after a few years. Many times we were in trouble after disturbing the neighbours, but were fortunate never to cause serious injury. I often found myself in trouble with my parents when someone was hurt, but despite the minor punishments, I know my parents were quite proud of my ingenuity.
Occasionally my father, Bob, was on the receiving end of my “brilliant” work. Observing a fraying cord on his electric drill, I repaired it but accidentally swapped the neutral and earth wire. He jumped rather high when he tried to use it a few days later while standing on wet grass. On another occasion my brothers decided to fly lighter-than-air balloons for our team at the school sports carnival. Since helium was not available, we built a device which pressurised domestic house gas and filled the balloons. Our technology was rather primitive however and these balloons contained quite a bit of air as well, but they did float satisfactorily. My father recognised this and warned us that they might be a little dangerous if they came in contact with an open flame. As an example, he demonstrated the risk by touching a lighted cigarette to one of the balloons as it floated under the back patio. He was enveloped in a ball of flame and his eyebrows were singed off. This did not worry us very much because we had seen him in this state before as he often seemed to be washing engine parts in gasoline and then testing the spark plugs of engines nearby.
After high school, at Newman College, although interested in science and mathematics, I felt that my mathematical ability was not strong enough to do electrical engineering, so I chose medical school as an alternative which was at least as interesting, and which did not require daily exposure to calculus! In addition the opportunity to study biological sciences was an attraction, particularly biochemistry which was not available in high school.
I met my wife Adrienne, a psychology student, at the University of Western Australia and we married in 1972 while I was doing my fifth year in medicine. I graduated from the University MBBS (Bachelor of Medicine, Bachelor of Surgery) in 1975 and thereafter performed internship and residencies in internal medicine at the Queen Elizabeth II Medical Centre (Sir Charles Gairdner Hospital). In those days I had no definite goals in medicine, but was interested in all aspects of clinical medicine including geriatrics, oncology and rheumatology. I was more interested in an academic career combining research with clinical medicine in a university hospital environment. I began my training as a specialist physician in 1978. In 1979 I moved to Royal Perth Hospital in order to become more experienced with cardiology and open heart surgery, which was only performed at that hospital in Perth.
Although we didn’t appreciate it at the time, my wife Adrienne and I must have been very busy during those years. We had four children, Luke, born in 1973, Bronwyn in 1975, Caroline in 1978 and Jessica in 1981. Adrienne was finishing the honours year of her psychology degree as Luke was being born. She was working in-between babies as a counsellor with the Education Department. My non-medical time was spent delivering children to various child-minding facilities, renovating our house, and indulging in my hobby of computers and electronics.
In the second half of 1981, my rotation took me to the gastroenterology division. It was there that I met Robin Warren. As part of my training I was encouraged to perform a clinical research project each year. I was already totally engrossed in a study of heat stroke in “fun runners” and might have progressed to sports or environmental medicine from there. However, I asked my boss, Dr Tom Waters, if there was a gastroenterology project I could start. He told me that Robin Warren had given him a list of patients with curved bacteria present on their stomach biopsies and needed someone to follow-up the patients to see what clinical diseases they had. I was especially interested because one of the people on Robin’s list was a woman I had seen in my ward, who had severe stomach pain but no diagnosis. In desperation we had referred her to a psychiatrist and commenced antidepressant medication for want of a better treatment. The only abnormal finding had some redness in the stomach and Robin’s bacteria on the stomach biopsy.
So I called Robin in the basement area of Royal Perth Hospital where the Pathology Department resided. It was to be the first of many afternoon visits in the next year. In those days, Robin used to drink strong black coffee and smoke small cigars, “cigarillos” I believe they were called. I too used to indulge occasionally, and would try out one of Robin’s cigars from time to time during our meetings. In our first meeting, Robin showed me slides of the curved bacteria he had seen, and explained the histopathology of the gastric mucosa to me.
I am often asked what made me listen to Robin and take up the research with him. Clearly this was an interesting thing to study, previously undescribed bacteria living in the acid-filled stomach. But I may have had other advantages compared with colleagues Robin had approached over the previous two years.
I was undifferentiated in that I wasn’t coming from a background in gastroenterology so that my knowledge and ideas were founded in general medical basic science rather than the dogma one was required to learn in specialist medicine. As a trainee general physician with broader training, I was comfortable with the notion of infectious disease and antibiotic therapies. I am told by others that I have a lateral thinking broad approach to problems, sometimes to my detriment. In school my grades always suffered because I was continually mucking about with irrelevant side issues which I often found to be more interesting.
At around that time also, I was aware of publications in the literature describing Campylobacter jejuni as a newly discovered common cause of food-borne gastroenteritis and colitis. Thus, I had seen pictures of campylobacters and could identify that Robin’s organisms appeared to be quite similar. In retrospect, one advantage of doing this research in Perth was that, as a modern Western society, H. Pylori was already in decline by 1981, so that rather than 80% of persons having the CLO, bacteria were only present in 30–50%. Thus, in any biopsy collection taken that year, Robin could see both infected specimens with inflammation (gastritis) and uninfected specimens which hardly ever had gastritis i.e. a “control group”. A further advantage I did have in 1981 was the new connection we had from the medical library to the National Library of Medicine at the NIH (Medline). Perhaps because of my interest in computer programming, this resource appealed to me and enabled me to enlist the librarians at Royal Perth Hospital to extensively search the past and current literature on gastric bacteria.
By the end of that first afternoon with Robin I was very interested. Over the next six months I followed the literature from book chapters, to their references, to deeper references, to material in library archives. I found that spiral gastric bacteria had been reported again and again but passed over. I could see an interesting paper being produced, perhaps in an obscure microbiological journal, but had no idea at the time of what we were really about to discover.
At the end of 1981, my gastroenterology term had almost finished and my term allocations for 1982 had been chosen. In the midst of all this time consuming and interesting research work I was still a physician in training. I was fitting in the research around education and patient commitments. In the first 6 months of 1982, I was to be a haematology registrar looking after the bone marrow transplant patients. In the second 6 months I was to be the physician at Port Hedland Hospital, a rotation to a point 2,000 kilometres north of Perth which attracted “hardship bonus”, i.e. $5,000 extra over 6 months. By then, I was very excited about the spiral bacteria. I had developed a degree of confidence in our methodology, and believed that we could safely carry out a study on 100 or so patients. I was able to keep the work going, continuing the research by fitting it around my other duties.
In November 1981, Adrienne had delivered our fourth child, Jessica. I was beginning a project which would occupy every minute of my spare time for the next 6 months. Adrienne was on maternity leave and was full time at home. It meant I could leave much of the parenting to her. We never did find the time to complete our home renovations and at the last minute in 1986 took out an extra home loan to pay someone to finish it for us. We had to have it in a rentable condition while we were in the USA.
I was fortunate to have a partner who was as enthusiastic about the work as I was. She also enjoys a challenge and shares my sense of adventure. Adrienne’s background in Psychology and experimental research was invaluable and she was always around to discuss the design of studies and the results of various other research works I had found. Over the years we took lots of chances. I took jobs on inadequate pay for many years. As my contemporaries were making their careers and achieving success I seemed to be falling further behind. I always had Adrienne’s full support. When she urged caution or vetoed some of my excesses, I knew it was time to really listen and re-evaluate. As time went on she became by my unofficial editor. All my early papers were edited by her and she helped with much of the discussion. Her liberal arts background means she is a more fluent writer than I. Over the past 25 years she has also helped to write and edit most of my books and speeches. All of the talks and speeches given in Stockholm were written with her substantial help.
My hobby of electronics was also an important aid in my research. In the evenings during 1981, I continued with my hobby of computing and electronics, so that by the end of that year I had completed the construction of a home computer capable of word processing. I was able to type grant proposals, consent forms and protocols. I was always on the leading edge of technology and my communication with overseas researchers was efficient because of that. It also meant I was able to access information not readily available. By 1981 I could function better as a single unfunded scientist than many units with multiple support staff.
The family moved to Port Hedland in July 1982 and I took all my references and textbooks with me. It was an important period. I had time to do an extensive literature search by correspondence and also had time to digest the results of our study and write it up for presentation. It was a great time for the family too. Winter in Port Hedland was beautiful, every day sunny with a temperature in the 80’s. We had a bit of extra money and we spent many weekends travelling in remote communities and camping with the kids under the stars.
In October 1982, I presented the preliminary findings from our study to the local College of Physicians meeting, where it received a mixed response. I found that my contract at Royal Perth would not be renewed the following year. I had successfully completed my training as a physician and now wanted to work in gastroenterology or microbiology to continue the work. These jobs at Royal Perth were not available.
Fortune stepped in when I was approached by Drs. Norm Marinovich and Ian Hislop at Fremantle Hospital who suggested they would find me a senior registrar position and fund me to continue. Fremantle is the third and smallest of the teaching hospitals in Perth and has a tradition of openness and experimentation. In the next two years at Fremantle I had an enthusiastic group of people working with me. Dr Ian Hislop, Norm Marinovich, Harvey Turner, David McGechie, Ross Glancy, Neil Noakes, Graeme Francis, Peter Rogers, Neil Stingemore, as well as great support from the Medical Superintendent, Peter Smith. The only downside of the appointment was that I was forced to halt my collaboration with Robin Warren. Robin did not have an appointment at Fremantle so the pathologist there, Ross Glancy, joined the team.
They were happy and very productive years. I was able to confirm very quickly that our observations of the bacteria at Royal Perth Hospital also applied in other parts of the city, the majority of peptic ulcer patients having the organism. I was still officially unfunded. The hospital was picking up all the costs of my work. It was at Fremantle in those two years that the first effective treatments were devised. I solved the conundrum of why bismuth has been such an effective stomach treatment for the past 200 years. I did my famous self experimentation and the early urease tests were developed.
A great piece of luck in early 1983 was finding Dr Martin Skirrow in the UK. I got his phone number from David McGechie. Skirrow arranged for the first presentation at the European Campylobacter Meeting in September 1983. Harvey Turner arranged a travel grant to take me to Brussels and the Gist Brocades Company, helped so that I could extend the trip, visit Martin in the UK and Guido Tytgat’s group in Amsterdam.
In September 1983, I visited Martin Skirrow in Worcester England, and attended an endoscopy session at the Worcester Infirmary. Martin’s registrar, Cliodna McNulty, was able to successfully isolate the organism 3 days later, showing that the spiral bug was not merely an Australian phenomenon but was present in ulcer patients in the UK as well. Martin Skirrow in Britain and Adrian Lee in Sydney were enormously encouraging, helping me with the microbiology in those early years.
In 1984 therefore, there were several groups around the world obtaining results which paralleled those of our group in Perth. In Australia, Adrian Lee in Sydney with Stuart Hazel and Hazel Mitchell also Nick Talley, John Lambert and Tom Borody were early researchers who made significant advances in the H. Pylori work. After the Brussels meeting, a core of researchers in Europe immediately picked up the research and much of the most important work on HP has been done by that group: my old friends, Mario Quina in Portugal, Tony Axon and Ashley Price in the UK, Francis Megraud in France, Peter Malfertheiner in Germany, Manuel Lopez Brea and Jose Pajares Garcia in Spain, Penti Sipponen in Finland, Dino Vaira and Giovanni Gasparini in Italy, Colm O’Morain in Ireland, Leif Andersen in Denmark, Alexander Hirschl in Austria, Guido Tytgat, Ernst Kuipers and Erik Rauws in The Netherlands, Michel Deltenre in Belgium, Pierre Michetti in Switzerland, Torkel Wadstrom and Lars Engstrand in Sweden. We became a closely knit group. The European group grew out of the campylobacter group I had met in Brussels in 1983 and today I count the members of that group amongst my closest friends. We have shared a remarkable story together.
In the USA David Graham, Pete Peterson and Martin Blazer began as critics. They set out to disprove the hypothesis but quickly became leaders in the field of HP research in the USA. With Tadetaka (Tachi) Yamada, although he was not directly involved in the HP research, they played an important role in moving various bodies such as the NIH towards action and acceptance of HP as an ulcer cause. In Asia, Takashi Shimoyama, Ken Kimura, Susumu Okabe, Yoshihiro Fukuda, Toshio Fujioka, Bow Ho, and K.L. Goh, were doctors who I was in contact with through the 1980s. They were developing their own HP research and supporting mine. In Asia, the H. Pylori research was taken up very quickly and I made my first visit to Japan in 1985 to present my work. There are too many others to list here. Needless to say, reports that I was alone in the promotion of HP as a pathogen are somewhat exaggerated.
But 1984 was a difficult year. I was unsuccessfully attempting to infect an animal model. There was interest and support from a few but most of my work was rejected for publication and even accepted papers were significantly delayed. I was met with constant criticism that my conclusions were premature and not well supported. When the work was presented, my results were disputed and disbelieved, not on the basis of science but because they simply could not be true. It was often said that no one was able to replicate my results. This was untrue but became part of the folklore of the period. I was told that the bacteria were either contaminants or harmless commensals.
At the same time I was successfully experimentally treating patients who had suffered with life threatening ulcer disease for years. Some of my patients had postponed surgery which became unnecessary after a simple 2 week course of antibiotics and bismuth. I had developed my hypothesis that these bacteria were the cause of peptic ulcers and a significant risk for stomach cancer. If I was right, then treatment for ulcer disease would be revolutionized. It would be simple, cheap and it would be a cure. It seemed to me that for the sake of patients this research had to be fast tracked. The sense of urgency and frustration with the medical community was partly due to my disposition and age. However, the primary reason was a practical one. I was driven to get this theory proven quickly to provide curative treatment for the millions of people suffering with ulcers around the world.
Becoming increasingly frustrated with the negative response to my work I realized I had to have an animal model and decided to use myself. Much has been written about the episode and I certainly had no idea it would become as important as it has. I didn’t actually expect to become as ill as I did. I didn’t discuss it with the ethics committee at the hospital. More significantly, I didn’t discuss it in detail with Adrienne. She was already convinced about the risk of these bacteria and I knew I would never get her approval. This was one of those occasions when it would be easier to get forgiveness than permission. I was taken by surprise by the severity of the infection. When I came home with my biopsy results showing colonization and classic histological damage to my stomach, Adrienne suggested it was time to treat myself. I had a successful infection, I had proved my point.
At the end of 1984 I was funded by the Australian Medical Research Council to conduct a prospective double blind trial to see if antibiotics could cure duodenal ulcers. It was conditional on getting a large number of patients into the study so I decided to move back to Royal Perth Hospital where the patient load is far higher. It meant I would be leaving my Fremantle colleagues and it was with some reluctance that I moved. When I returned to Australia in 1996, I was asked to be Patron of the Fremantle Hospital Research Foundation and I take great pride in having that position. At Royal Perth I was again working with Robin, John Armstrong, Len Matz, John Pearman, Stewart Goodwin, Doug Annear and Helen Royce.
Even though I was not officially collaborating with Robin when I was working at Fremantle Hospital in 1983–84, we still met to discuss the papers we were writing for the Lancet and would meet for dinner with our wives. We had one of these dinners only a few weeks after my self experimentation experiment. I was enthusiastic about the results and the severity of my illness. It was also the first confirmation of infection with documented results. I was eager to share the news with Rob and he was equally excited about it. Early the next morning he had a call from a journalist in the USA at 5 am who had his timing totally off. No one is ever able to figure out what time it is in Perth. When asked the usual question about “How do you know it’s a pathogen and not a harmless commensal?” Rob blabbed the results of my still unreleased work with “I know because Barry Marshall has just infected himself and damn near died”; a slight exaggeration, but it made for good copy. What he didn’t know was that the journalist he was speaking to was from the “Star” newspaper, a tabloid that often features with stories about alien babies being adopted by Nancy Reagan. This was right up their alley. The next day the story appeared, “Guinea-pig doctor discovers new cure for ulcers … and the cause.”
This became one of the serendipitous, life changing events in my life and I have Rob’s temper to thank for it. Firstly, I was contacted by a continuous line of patients in the USA who read the story and were desperate for treatment. I was able to help. I was treating patients by proxy in the USA as early as 1984.
Ten years later this became important in a dispute with another doctor who claimed to be the first. I still had the records from some of these patients and was able to get in touch with them to prove my claim to be first.
The second result was that it was read by Mike Manhart, a microbiologist working for Proctor and Gamble in the USA. He tracked down my published letters and realized the economic potential for P & G who made a bismuth drug and set up a business relationship. P & G later patented much of my work and also helped me with patents on my diagnostics. There was little money in any of this for the first 10 years but after 1995 it became a significant income for us. P & G funded a fellowship for me in the USA to replicate and push the research there. We departed Australia, believing that it shouldn’t take more than 2–3 years to convince the world that antibiotics would cure most gastric diseases.
It also brought Bruce and Claudette McCarty into my life. Bruce was head of Health and Personal Care products at P & G and became an important mentor. He arranged support funding to set up a lab at University of Virginia. Bruce became a good friend and a keen advocate for H. Pylori research in the USA. He taught me a lot about how business works best in a trusting and responsible way to benefit everyone. It also seemed to me that he and Claudette spent lots of time in their life just having fun with family and friends. Tragically, Bruce died in 2004. It was a great sadness for me and Adrienne that he and Claudette were not there in Sweden to see me receive the Prize. He always believed in me and his faith in the work and great enthusiasm never failed.
The ten years spent at University of Virginia, were a chance to extend my research, particularly in the area of treatment and diagnostics. I became an advocate for treatment though many called me a zealot. They were often hard years for the family particularly the first few years when we were on a financial shoestring. They were rewarding as well. I had continuous stream of letters from patients who had been treated and freed from a lifetime of pain and disruption. I worked with a great team at UVA. Richard McCallum was head of Gastroenterology and Dick Guerrant in Infectious Diseases. McCallum gave me free rein and sponsored my academic rise in the USA. I also did great collaborative work with Dick over the years. David Peura, a long-time H. Pylori enthusiast from the US Army, moved to UVA in 1992. My team included nurse Susie Hoffman, nuclear technician Michael Plankey, post-doc Matthew Coombs, data manager Linda Mosen, programmer Sherry Boyd, assistant Nancy Noblette and many others. We were regarded as being outside the mainstream but were a great enthusiastic group and became lifelong friends.
I also met Bill and Sandy Fry in 1987. Bill owned a company Tri-Med along with Phil Patterson and Kevin Dye. Bill Fry bankrolled a USA study for my CLOtest diagnostic and launched it in the USA. Later he was to also pick up the C14-Urea Breath Test and shepherded it through the FDA at a cost of several million dollars. I count Bill amongst my closest friends, a brilliant salesman and an example of a team leader. No matter how black things looked, Bill could always find a silver lining for us even though I am certain he was secretly concerned about our chances of success. Bill’s credo which he lives by is that “Good things happen to good people”. We have done a lot of good stuff together and had many great times.
Patients often wanted to make a donation to the work so I set up a foundation to use the money for patient and doctor education about the research. On one occasion there had been a story about the cure in the Sunday papers across the USA. In the following weeks we received 30,000 letters all with donations of a dollar or two to pay for postage and photocopying of information. We had to hire in students to handle it all.
Over the years the journalists who covered the story helped significantly in educating the public to ask for and later demand the new treatments from unwilling doctors. Suzanne Chazin in the Readers Digest, Terry Monmany in the New Yorker, Mark Ragg in the Bulletin and Larry Altman in the New York Times all wrote detailed reviews of the work that became important sources of information. The BBC show Ulcer Wars produced by Michael Mosley is still shown around the world.
The tide of acceptance began to turn in the early 1990s and by 1992 I could go to meetings and receive as much praise as criticism. 1994 was a watershed year for us. In February 1994 the NIH held a consensus meeting in Washington DC which ended after 2 days with the statement to the effect that the key to treatment of duodenal and gastric ulcer was detection and eradication of Helicobacter pylori.
I had been waiting for ten years for this day and I felt a combination of relief and satisfaction that I had achieved what I set out to do. Years before, I had developed the hypothesis, tested it, proved it and now it had reached official acceptance.
The next year proved to be harder. I began to receive awards and recognition. At the hospital, I was still carrying a full load of patient care and research. However, I was increasingly dissatisfied. Much of my time was being spent attending meetings and travelling. I think the pressure of the previous 10 years was beginning to show. Because I had been so involved in the exponential rise of Helicobacter, I had been unable to update my training in new areas of molecular biology which by then were coming to represent a large proportion of the Helicobacter publications.
In typical fashion Adrienne took over the decision-making and at the end of 1994, I took a year of leave from the university. We cashed in my superannuation and decided to live on that for a year to figure out what would be next in our lives. In that year I still travelled and lectured but my primary work was with Tri-Med, getting the breath test through the FDA regulatory process. I am proud of my diagnostics tests, the CLOtest and PYtest. They are often my forgotten children, eclipsed by my work on treatment. Although less glamorous than high impact papers, reliable cheap and available diagnostics are just as important in medicine as treatments. They don’t always get the same recognition. After 1994 my business interests became more important. The diagnostics were starting to earn an income. In Australia, close friend Rod Blechynden took on the role of managing it for me. Rod and Adrienne take care of the business aspects of my work. Their work frees me to focus on my research.
Once I had completed that project, Adrienne decided it was time for us all to go home. I was still unsure but it has turned out to be the best decision for me and the family. We moved back to Perth in 1996. I was awarded the McFarlane Burnet Fellowship which funded my lab at the University of WA for a 5 year period. In 1998, Tri-Med USA bought the manufacturing rights to CLOtest. I was keen to keep the manufacturing in Western Australia. It has been a long term ambition of mine to develop industry here in Perth. I set up a new manufacturing facility here but, sadly, it didn’t last. Tri-Med in the US was later sold and the new owners moved all the manufacturing back to the USA. Tri-Med in Perth continues in a small way doing R&D and selling medical products.
Before finishing I want to acknowledge all those scientists who failed to recognize HP. Without them I would have had a very different career. Some of their stories are described in my book “Helicobacter Pioneers”. I also want to thank Irvin Modlin for the foreword he wrote for it. He is a great guy and was able to say things about the joy of scientific research that I never could.
One of the truly great things about winning the Nobel Prize in 2005 was that I was living and working back home. I got to share it and celebrate with those who had been involved in the initial work at Royal Perth and Fremantle Hospital.
I continue to live in Perth Western Australia. I have an appointment at The University of Western Australia and still see patients at the gastroenterology department at Sir Charles Gairdner Hospital. My other interests continue. I take an active role in Tri-Med and in 2005 began a new project with vaccine company Ondek.
There were many occasions when luck played a role in my life; meeting with Robin, the first culture of the bacteria and chance meetings with many people who helped me and collaborated with me. I look back and am grateful to the many friends and family who helped me along the way, most importantly, my wife Adrienne, and my children, their partners and my grandchildren.
Barry James Marshall AC FRACP FRS FAA[1][2] (born 30 September 1951) is an Australian physician, Nobel Prize Laureate in Physiology or Medicine, Professor of Clinical Microbiology and Co-Director of the Marshall Centre[4] at the University of Western Australia.[5] Marshall and Robin Warren showed that the bacterium Helicobacter pylori (H. pylori) plays a major role in causing many peptic ulcers, challenging decades of medical doctrine holding that ulcers were caused primarily by stress, spicy foods, and too much acid. This discovery has allowed for a breakthrough in understanding a causative link between Helicobacter pylori infection and stomach cancer.[6][7][8]Contents1 Education and early life2 Career and research3 Awards and honours4 See also5 References6 External linksEducation and early lifeMarshall was born in Kalgoorlie, Western Australia and lived in Kalgoorlie and Carnarvon until moving to Perth at the age of eight. His father held various jobs, and his mother was a nurse. He is the eldest of four siblings. He attended Newman College for his secondary education and the University of Western Australia School of Medicine, where he received a Bachelor of Medicine, Bachelor of Surgery (MBBS) in 1974.[1] He married his wife Adrienne in 1972 and has four children.[9][10][11]
Career and researchIn 1979, Marshall was appointed Registrar in Medicine at the Royal Perth Hospital. He met Dr. Robin Warren, a pathologist interested in gastritis, during internal medicine fellowship training at Royal Perth Hospital in 1981. Together, the pair studied the presence of spiral bacteria in association with gastritis. In 1982, they performed the initial culture of H. pylori and developed their hypothesis on the bacterial cause of peptic ulcers and gastric cancer.[9] It has been claimed that the H. pylori theory was ridiculed by established scientists and doctors, who did not believe that any bacteria could live in the acidic environment of the stomach. Marshall was quoted as saying in 1998 that "everyone was against me, but I knew I was right."[12] On the other hand, it has also been argued that medical researchers showed a proper degree of scientific scepticism until the H. pylori hypothesis could be supported by evidence.[13]
In 1982 Marshall and Warren obtained funding for one year of research. The first 30 out of 100 samples showed no support for their hypothesis. However, it was discovered that the lab technicians had been throwing out the cultures after two days. This was standard practice for throat swabs where other organisms in the mouth rendered cultures unusable after two days. Due to other hospital work, the lab technicians did not have time to immediately throw out the 31st test on the second day, and so it stayed from Thursday through to the following Monday. In that sample, they discovered the presence of H. pylori. They later found out that H. pylori grow more slowly than two days, and the stomach cultures were not contaminated by other organisms.[14]
In 1983 they submitted their findings thus far to the Gastroenterological Society of Australia, but the reviewers turned their paper down, rating it in the bottom 10% of those they received that year.[14]
After failed attempts to infect piglets in 1984, Marshall, after having a baseline endoscopy done, drank a broth containing cultured H. pylori, expecting to develop, perhaps years later, an ulcer.[15] He was surprised when, only three days later, he developed vague nausea and halitosis, due to the achlorhydria. There was no acid to kill bacteria in the stomach and their waste products manifested as bad breath), noticed only by his mother. On days 5–8, he developed achlorhydric (no acid) vomiting. On day eight, he had a repeat endoscopy, which showed massive inflammation (gastritis), and a biopsy from which H. pylori was cultured, showing it had colonised his stomach. On the fourteenth day after ingestion, a third endoscopy was done, and Marshall began to take antibiotics.[16] Marshall did not develop antibodies to H. pylori, suggesting that innate immunity can sometimes eradicate acute H. pylori infection. Marshall's illness and recovery, based on a culture of organisms extracted from a patient, fulfilled Koch's postulates for H. pylori and gastritis, but not for peptic ulcers. This experiment was published in 1985 in the Medical Journal of Australia[17] and is among the most cited articles from the journal.[18]
After his work at Fremantle Hospital, Marshall did research at Royal Perth Hospital (1985–86) and at the University of Virginia, USA (1986–present), before returning to Australia while remaining on the faculty of the University of Virginia.[3] He held a Burnet Fellowship at the University of Western Australia (UWA) from 1998–2003.[19] Marshall continues research related to H. pylori and runs the H. pylori Research Laboratory at UWA.[20]
In 2007, Marshall was appointed Co-Director of The Marshall Centre for Infectious Diseases Research and Training, founded in his honour. In addition to Helicobacter pylori research, the Centre conducted varied research into infectious disease identification and surveillance, diagnostics and drug design, and transformative discovery. His research group expanded to embrace new technologies, including Next-Generation Sequencing and genomic analysis. Marshall also accepted a part-time appointment at the Pennsylvania State University that same year.[21] In August 2020, Marshall, along with Simon J. Thorpe, accepted a position at the scientific advisory board of Brainchip INC, a computer chip company.[22]
Awards and honoursIn 2005, the Karolinska Institute in Stockholm awarded the Nobel Prize in Physiology or Medicine to Marshall and Robin Warren, his long-time collaborator, "for their discovery of the bacterium Helicobacter pylori and its role in gastritis and peptic ulcer disease".[23]
Marshall also received the Warren Alpert Prize in 1994; the Australian Medical Association Award and the Albert Lasker Award for Clinical Medical Research in 1995; the Gairdner Foundation International Award in 1996; the Paul Ehrlich and Ludwig Darmstaedter Prize in 1997; the Golden Plate Award of the American Academy of Achievement,[24] the Dr A.H. Heineken Prize for Medicine, the Florey Medal, and the Buchanan Medal of the Royal Society in 1998.
He was elected a Fellow of the Royal Society (FRS) in 1999. His certificate of election to the Royal Society reads:[2]
Barry Marshall, together with Robin Warren, discovered spiral bacteria in the stomachs of almost all patients with active chronic gastritis, or duodenal or gastric ulcers, and proposed that the bacteria were an important factor in the aetiology of these diseases. In 1985, Marshall showed by self-administration that this bacterium, now called Helicobacter pylori, causes acute gastritis and suggested that chronic colonisation directly leads to peptic ulceration. These results were a major challenge to the prevailing view that gastric disorders had a physiological basis, rather than being infectious diseases. Marshall showed that antibiotic and bismuth salt regimens that killed H. pylori resulted in the cure of duodenal ulcers. The view that gastric disorders are infectious diseases is now firmly established and there is increasing evidence for a role of H. pylori infection in gastric cancers. The work of Marshall has produced one of the most radical and important changes in medical perception in the last 50 years. Barry Marshall was awarded the Albert Lasker Award for Clinical Science in 1995 and the Buchanan Medal in 1998.
Marshall was awarded the Benjamin Franklin Medal for Life Sciences in 1999; the Keio Medical Science Prize in 2002; and the Australian Centenary Medal and Macfarlane Burnet Medal and Lecture in 2003.[25][26]
Marshall was appointed a Companion of the Order of Australia in 2007.[27] He was awarded an honorary Doctor of Science degree by the University of Oxford in 2009.[28]
Marshall was elected Fellow of the Australian Academy of Health and Medical Sciences (FAHMS) in 2015.[29]
Marshall was awarded the honour of Western Australian of the Year in 2006.[30]
Marshall was awarded The Companion in the General Division of the Order of Australia (AC) in 2007.[31]
Marshall was awarded The University of Oxford honorary Doctor of Science degree in 2009.[32]
Marshall in the Ambassador for Life Sciences for Western Australia.
Related Items:
Alfred Nobel Peace Prize Medal Coin
$25.00
"Nobel Prize in Economics" Tjalling Koopmans Clipped Signature
$199.99
"Nobel Prize for Chemistry" Ahmed Zewail Signed Nobel Pamphlet
$199.99