Researchers have identified a new method of attack on the brain’s neurologic functions that appears to be employed by a whole range of neurodegenerative diseases such as HIV dementia, Alzheimer’s, multiple sclerosis and Parkinson’s. The study, appearing in The Journal of Clinical Investigation, describes how when inflammation occurs in the brain, nerve impulses that are passed between cells during routine activities like learning and memory can become toxic. Instead of triggering the normal neurological function – such as the formation of memories – the impulses can inflict injury on neurons and disrupt the functioning of the brain.
One of the previous suspects in neurodegenerative disease has been glutamate, an amino acid that normally acts as a neurotransmitter. However, excess glutamate can overly excite neurons, causing damage and death – a process called excitotoxicity.
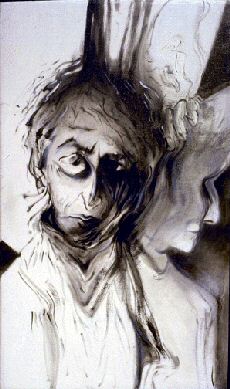
The researchers’ attention turned to dendrites, the crooked branches of neurons that carry impulses toward the body of the nerve cell, and synapses, the places where impulses pass from neuron to neuron. Injury to dendrites – characterized by swelling or beading, loss of dendrite spines, and reduction in size – is seen in HIV dementia and Alzheimer’s.
Experiments were then carried out where brain cells were exposed to platelet-activating factor, a compound that promotes inflammation and plays many roles in the brain. It can be produced by neurons and takes part in the working of synapses, including activity associated with learning and remembering. It also is produced by immune cells during inflammation. The amount of platelet-activating factor in the brain increases dramatically in HIV-1-associated dementia and other neurodegenerative diseases.
The results showed that elevated levels of platelet-activating factor promoted beading on dendrites and injury to synapses following bursts of synaptic activity similar to those thought to be involved in learning and memory. Co-researcher Matthew J. Bellizzi explained further. “We found that disease makes dendrites more vulnerable to excitotoxicity. We also found that damage to the dendrites may not require abnormal glutamate exposure.”
Gelbard explained that this new mechanism was used by a number of diseases. “It applies to Alzheimer’s, multiple sclerosis, Parkinson’s and any neurodegenerative diseases that have synaptic dysfunction with inflammation, which is virtually all of them.”
The researchers, from the University of Rochester Medical Center and University of California at San Diego, said that the new understanding of this process could provide a new path for drugs to treat the diseases. As a first step in this direction, the scientists propose a strategy of chemical preconditioning to induce adaptations in nerve cells that would enable the cells to better withstand toxic attacks, prevent injury and preserve function. “Preconditioning would allow the nervous system to experience stress and become more resistant to future encounters with stress and the damage it can trigger,” said Gelbard.
The researchers have been examining one particular drug – diazoxide – to assess its potential to precondition brain cells. In lab studies, brain cells treated with diazoxide before exposure to the platelet-activating factor prevented dendritic beading and preserved synaptic functions. “Stressing the cells with small amounts could trigger protective genes and induce adaptations that will make the dendrites more able to withstand insults,” Bellizzi said.
“Preconditioning to protect the synapse is likely to be more important in the early and middle phases of neurodegenerative diseases than simply preserving the cell body,” Gelbard concluded.








Comments are closed.