
University of California, San Diego (UCSD) bioengineers have fabricated cartilage tissue which for the first time mimics the multi-layered structure and cellular functions of natural articular cartilage.
The tissue is made entirely from biological materials using a modification of a technique invented at Rush-Presbyterian-St. Luke’s Medical Center, Chicago. The researchers hope this tissue could be developed as an implant treatment for the millions of people who suffer from cartilage damage associated with joint injuries, congenital defects, arthritis and age-related degeneration.
Robert Sah, professor of bioengineering at the UCSD Jacobs School of Engineering, led the study, conducted by graduate students Travis Klein and Kelvin Li and staff researcher Barb Schumacher at UCSD, in collaboration with Professors Koichi Masuda and Eugene Thonar of Rush. Klein will describe the results at the Biomedical Engineering Society annual meeting at 2:15 p.m. on Saturday, October 6 at the Sheraton Imperial in Durham, North Carolina.
Cartilage is the body’s shock absorber, a cushion of durable tissue that protects the knee from a lifetime of walking, bending and running. Though just a few millimeters thick, cartilage is nevertheless quite complex, consisting of a surface, middle and deep region, each with its own distinct composition and structure.
In previous research, Sah detailed the mechanical properties of cartilage and found that it is soft at the surface, but 25 times stiffer in the deep regions. Meanwhile, Barbara Schumacher, then at Rush, found that the cells in the surface region make a key protein, called Superficial Zone Protein, which is a major lubricant of joints.
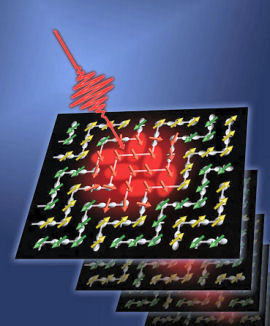
Using this data, bioengineers at UCSD developed a map for how to organize different types of chondrocytes to mimic the stratified nature of cartilage tissue. They then grew this cell mix together using the ARC (Alginate Recovered Chondrocyte) method developed at Rush, which suspends cells in a gel until the cells begin to form their own matrix or scaffolding. The gel is then removed, leaving an entirely biological tissue.
In laboratory tests, the researchers found that the cells at the surface of their engineered tissue effectively secreted the key molecule, Superficial Zone Protein, needed to lubricate the joint. In addition, the cells at the surface were making tissue that was softer and had a less dense matrix, while the cells in the deeper regions were spaced further apart and had a more densely packed matrix, which made the tissue stiffer.
The researchers believe that the engineered tissue will mature like cartilage does naturally in humans. During fetal development, cartilage cells are densely packed, and the matrix is loosely knit. But as a child grows and the matrix supporting the cartilage gets stronger, cartilage cells spread out. By the time an individual reaches adulthood, the cartilage is mature, the cells become less active, and the tissue is about four fold stiffer than during early development.
The engineered tissue is like immature cartilage, and the researchers believe this will give the implant an advantage because as it continues to mature, it is likely to integrate well and conform to fit with the patient’s surrounding cartilage and joint tissue.












Comments are closed.