42 page TRAUMATIC BRAIN INJURY Primer PowerPoint Presentation on CD For Sale
When you click on links to various merchants on this site and make a purchase, this can result in this site earning a commission. Affiliate programs and affiliations include, but are not limited to, the eBay Partner Network.
42 page TRAUMATIC BRAIN INJURY Primer PowerPoint Presentation on CD:
$12.99
Thank you!
If you do not wish to have your item(s) delivered on data disc(s), I can provide them on a flash drive and other means as well. Just let me know if a disc does not work for you and we can discuss delivery by other methods.
COMBINING SHIPPING COSTS
Are you purchasing multiple items? I will: a) combine all invoices before payment and charge shipping equivalent to one item, or b) refund all shipping costs in excess of one item after payment.
$3.00 first class shipping in U.S.Includes the Adobe Acrobat Reader for reading and printing publications.
Numerous illustrations and matrices.
Contains the following key public domain (not copyrighted) U.S. Government publication(s) on one CD-ROM in both Microsoft PowerPoint and Adobe Acrobat PDF file formats:
TITLE: Traumatic Brain Injuries: Pathophysiology, Treatment and Prevention, 42 pages (slides)
SLIDE TOPICS, SUBTOPICS and CONTENTS:
Traumatic Brain Injuries: Pathophysiology, Treatment and Prevention
Disclaimer The views expressed in this presentation are those of the author and do not reflect the official policy of the Department of the Army, Department of Defense, or U.S. Government.
Defense and Veterans Brain Injury Center (DVBIC)
DVBIC, founded in 1991 as the Defense and Veterans Head Injury Program (DVHIP), a congressionally funded DoD-VA Disease Management Program. The DVBIC mission:
conduct clinical research
ensure optimal clinical care
education for military, veterans, and their families.Military Sites: WRAMC, NMCSD, WH-BAMC
VAMC’s – Richmond, Minn, Palo Alto, Tampa
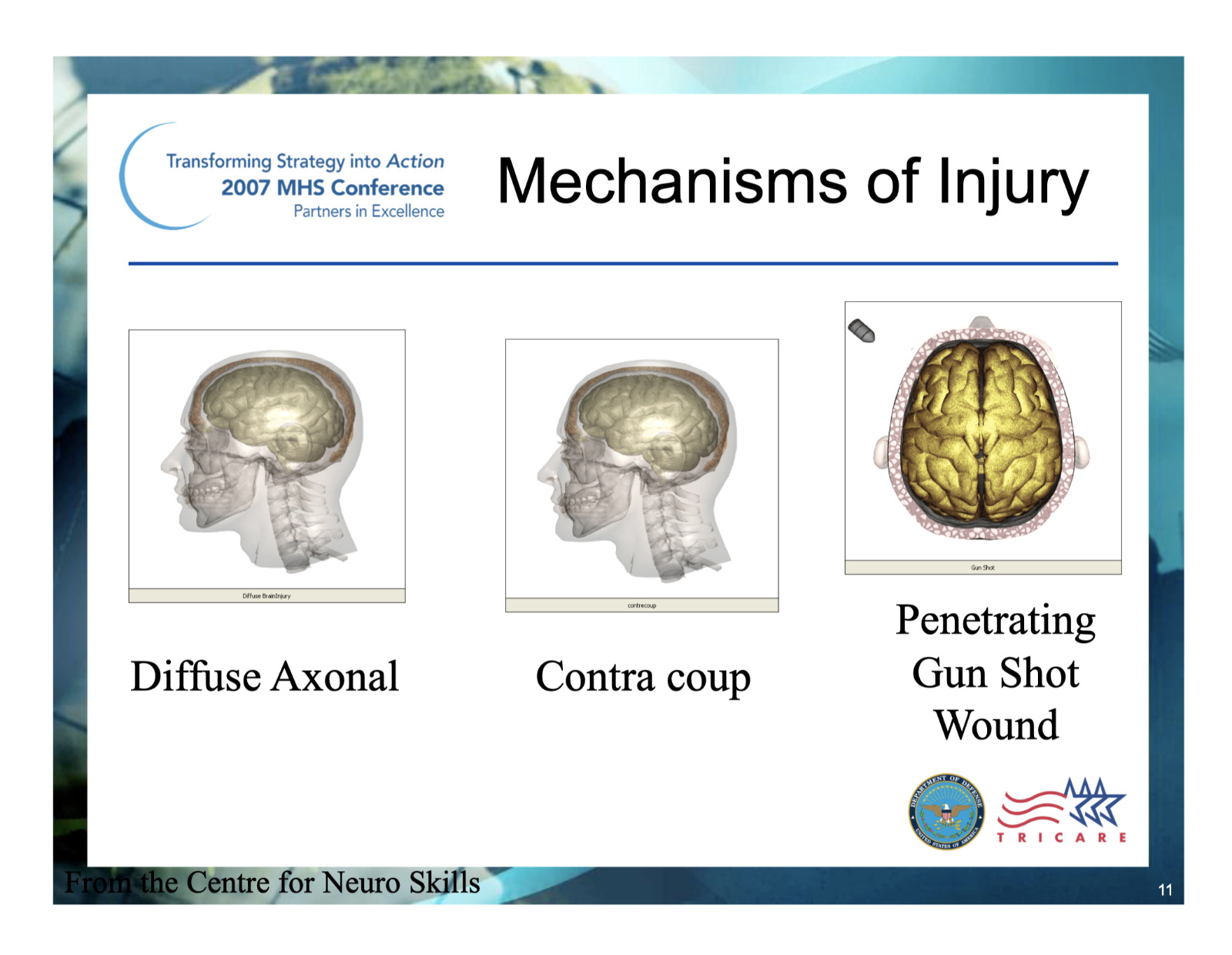
civilian community reentry programs – Virginia Neurocare and Laurel Highlands (Western Penna)Mechanisms of Injury
Traumatic Brain Injury Description
American Congress of Rehabilitation Medicine: Mild Traumatic Brain Injury (MTBI) Definition
A traumatically induced physiological disruption of brain function manifested by at least one of these symptoms:
Loss of consciousness < 30 minutes
Loss of memory for events immediately before (retrograde amnesia) or after the accident (Post Traumatic Amnesia <24 hours)
Any alteration in mental state at the time of the injury (dazed, disoriented, confused)
Presence of focal neurological deficits
If given, GCS score > 13
Kay, et al., 1993
Head Injury in the U.S. Military
Traumatic Brain Injury (TBI) Epidemiology: IncidenceMechanisms of InjuryPathophysiology of Injury
Primary Injury: Function of energy transmitted to brain
Very little can be done by health care providers to influence
Command enforcement of personal protection
Helmets, SeatbeltsSecondary Injury: Function of damage to brain from systemic physiology
Systemic
Hypotension: Acute and easily treatable
Hypoxia: Acute and easily treatable
Fever and Electrolyte Imbalances
Seizures
Intracranial Pressure Can Lead to Herniation
Neuropathology of Closed TBI
Primary Injury:
Contusions/Hemorrhages
Diffuse Axonal Injury (DAI)Secondary Injury (Intracranial):
Blood Flow and Metabolic Changes
Traumatic Hematomas
Cerebral Edema
Hydrocephalus
Increased Intracranial Pressure
Severe and Penetrating Brain Injury: Clinical Challenges
Craniectomy
Vascular Complications
47.4% had traumatic cerebral vasospasm. Majority were blast related injury (Armonda, R., Bell, R., Vo,A., et al 2006. Wartime traumatic cerebral vasospasm: Recent review of combat casualties. Neurosurgery, 59(6), 1215 -1225.)
Autonomic Instability/Sympathetic Storms
Infectious Complications Archives of Physical Medicine and Rehab (Invited Manuscript) R. Riechers, et al.
Brain-Behavior Relationships and Regional Cortical Vulnerability to TBI Figure adapted from Arciniegas and Beresford 2001) Post Concussive Symptoms in Mild TBI
Natural history is recovery within weeks/months (Levin 1987)A small percentage will have persistent symptoms (Alexander, Neurology 1995)Repeat concussions – more morofferity (Collins, et al, Neurosurgery 2002)Educational interventions effective in reducing symptoms (Ponsford, et al. 2002)Cognitive Changes
Attention/ConcentrationSpeed of Mental ProcessingLearning/Information Retrieval Executive Functions (e. g., Planning, Problem Solving, Self Monitoring) May see judgment problems, apathy, inappropriate behaviors
fMRI study of MTBI and Memory (McAllister, et al, 2000)
Neurometabolic Changes and Concussion (Hovda et al, 1998)
Simple Reaction Time Warden D, Bleiberg J, Cameron K, et al, Neurology, 2001
Concussion:Time to Recovery
Post Deployment TBI Questions
Did you have any injury(ies) during your deployment from any of the following? (check all that apply):
1. Fragment
2. Bullet
3. Vehicular (any type of vehicle, including airplane)
4. Fall
5. Blast (Improvised Explosive Device, RPG, Land mine, Grenade, etc.)
6. Other specify:
Did any injury received while you were deployed result in any of the following? (check
all that apply):
1. Being dazed, confused or “seeing stars”
2. Not remembering the injury
3. Losing consciousness (knocked out) for less than a minute
4. Losing consciousness for 1-20 minutes
5. Losing consciousness for longer than 20 minutes
6. Having any symptoms of concussion afterward (such as headache, dizziness, irritability, etc.)
7. Head Injury
8. None of the above (any of 1-5 suggest a MTBI diagnosis)
Post-Deployment TBI Screening
DVBIC has worked with multiple sites screening returning war fighters Approximately 10-20% war fighters had a TBI while in theater (Army Times-Sept 5, 2005)Virtually all were mild TBIMost are now asymptomatic
WRAMC TBI Screening Flow Chart
Walter Reed OIF/OEF TBI Experience (1/03 to 4/05)
N=433 Hospitalized patients with TBI
68% of injuries were due to explosion/blast
88.5% were closed TBI
Post Traumatic Amnesia (PTA) < 24 hours: 43%
Walter Reed OIF/OEF TBI Experience (cont.)
Complications - 14% shock; 9.5% hypoxia; 25% skull fracture; 18.7% subdural hematoma; and 1.5% epidurals
6% had seizures
19% had limb amputations; lower extremity most common
91 % reported post concussive symptoms:
headache (47%)
memory deficits (46%)
irritability/aggression (45%)
attention/concentration difficulties (41%)
Of 43% with a psychiatric symptoms noted, depression was the most
common (27%).
Military ContextEvaluation of MTBI in the field
Medic obtains history using
Military Acute Concussion Evaluation (MACE)
New Clinical Practice Guideline drawing on sports concussion and operational experts released 22 Dec 06– includes the SAC – Standard Assessment of Concussion (McCrea 2000)Conclusions Regarding PTSD in TBI Patients
Studies suggest that PTSD following TBI does occur, but may be modified by the brain injury. Intrusive memories are less common in individuals; when present, highly predictive of PTSDPTSD is more likely in mild TBI than severe TBI (Bombardier, C., et al. 2006. J Neuropsychiatry Clin Neurosci: Posttraumatic Stress Disorder Symptoms During the First Six Months After Traumatic Brain Injury: 18:4:501-508)Treatment Areas
Education and support for the patient’s family
Rest and avoidance of another injury
Individual and group therapies
Medication including symptom mgt
Rehab (acute, sub-acute, community re-entry)
Guidelines for the Pharmacologic Treatment of Neurobehavioral Sequelae of TBI
Symptom Management
Addresses 3 topic areas
Aggression
Cognitive disorders
Affective disorder/Anxiety/Psychotic disorders
Warden D., Gordon B., McAllister T., et al (2006). Guidelines for the pharmacologic treatment of neurobehavioral sequelae of traumatic brain injury. Journal of Neurotrauma, 10(23), 1468-1501.
Guidelines for the Pharmacologic Treatment of Neurobehavioral Sequelae of TBI
Despite reviewing a significant number of studies on drug treatment of neurobehavioral sequelae after TBI, the quality of evidence did not support any treatment standards and few guidelines due to a number of recurrent methodological problems. Guidelines were established for the use of methylphenidate in the treatment of deficits in attention and speed of information processing, as well as for the use of beta-blockers for the treatment of aggression following TBI. Options were recommended in the treatment of depression, bipolar disorder/mania, psychosis, aggression, general cognitive functions, and deficits in attention, speed of processing, and memory after TBI.
Prevention Areas
Rest to prevent re-injury
Education regarding risk taking behaviors
Neurometabolic changes and concussion
Helmets
Questions?DVBIC Headquarters, WRAMC
Amy Craig, MBA
Pannakal David, MD
COL James Ecklund, MC
Jamie Fraser, MPH
Louis French, PsyD
Phil Girard, MS
Kathy Helmick, RN, CRNP
Maraquita Hollman, BA
Ronnell Iandolo, RN
Angela Ibrahim, MPA, CRA
Brian Ivins, MA
COL Robert Labutta, MC
COL Geoff Ling, MCWei Lu, RN
Lisa Moy Martin, RNC
Silvia Massetti, MSW
Kathryn Misner, PA-C
Sonal Pancholi, PhD
Glenn Parkinson, MSW, MA
CPT Ron Riechers, MC
Karen Schwab, PhD
Alice Marie Stevens, MA
Katie Sullivan, MS
Jose Valls, LPN
Jehue Wilkinson, LPN
Michael Wilmore, PA-C
Cecilie Witt, BA
Related Items:
42 page TRAUMATIC BRAIN INJURY Primer PowerPoint Presentation on CD
$12.99
STAR WARS #42 1980 Marvel Comics CGC 5.0 Very Good/Fine White Pages KEY ISSUE
$265.99
Amazing Spider-man #42 CPA 7.5 SINGLE PAGE #6/7 2nd app. The Rhino
$79.99