68 page War TRAUMATIC BRAIN INJURY PowerPoint Presentation on CD For Sale
When you click on links to various merchants on this site and make a purchase, this can result in this site earning a commission. Affiliate programs and affiliations include, but are not limited to, the eBay Partner Network.
68 page War TRAUMATIC BRAIN INJURY PowerPoint Presentation on CD :
$12.99
Thank you!
If you do not wish to have your item(s) delivered on data disc(s), I can provide them on a flash drive and other means as well. Just let me know if a disc does not work for you and we can discuss delivery by other methods.
COMBINING SHIPPING COSTS
Are you purchasing multiple items? I will: a) combine all invoices before payment and charge shipping equivalent to one item, or b) refund all shipping costs in excess of one item after payment.
All derivative (i.e. change in media; by compilation) work from this underlying U.S. Government public domain/public release data is COPYRIGHT © GOVPUBS$3.00 first class shipping in U.S. and rest of world.
Includes the Adobe Acrobat Reader for reading and printing publications.
Numerous illustrations and matrices.
Contains the following key public domain (not copyrighted) U.S. Government publication(s) on one CD-ROM in both Microsoft PowerPoint and Adobe Acrobat PDF file formats:
TITLE: Traumatic Brain Injury
SLIDE TOPICS, SUBTOPICS and CONTENTS:
Traumatic Brain Injury
Objectives
Epidemiology of head injury
Review of pathophysiology
Discuss the clinical spectrum of traumatic brain injury (TBI)
Discuss presentation of specific types of head injuries
Discuss management
ObjectivesDiscuss new guidelines for screening mTBI patients
Discuss management of mTBI casualty
Scope of Problem
66% of wounded in OIF are from Blast InjuryOf soldiers exposed to a blast –
41% have evidence of TBIA 22 month study at Ft. Carson reported 1 in 6 Soldiers with some evidence of mild TBI (average of 18%).
Physiology
Cerebral dynamics
Uses 20% of O2 volume and 15% of cardiac output
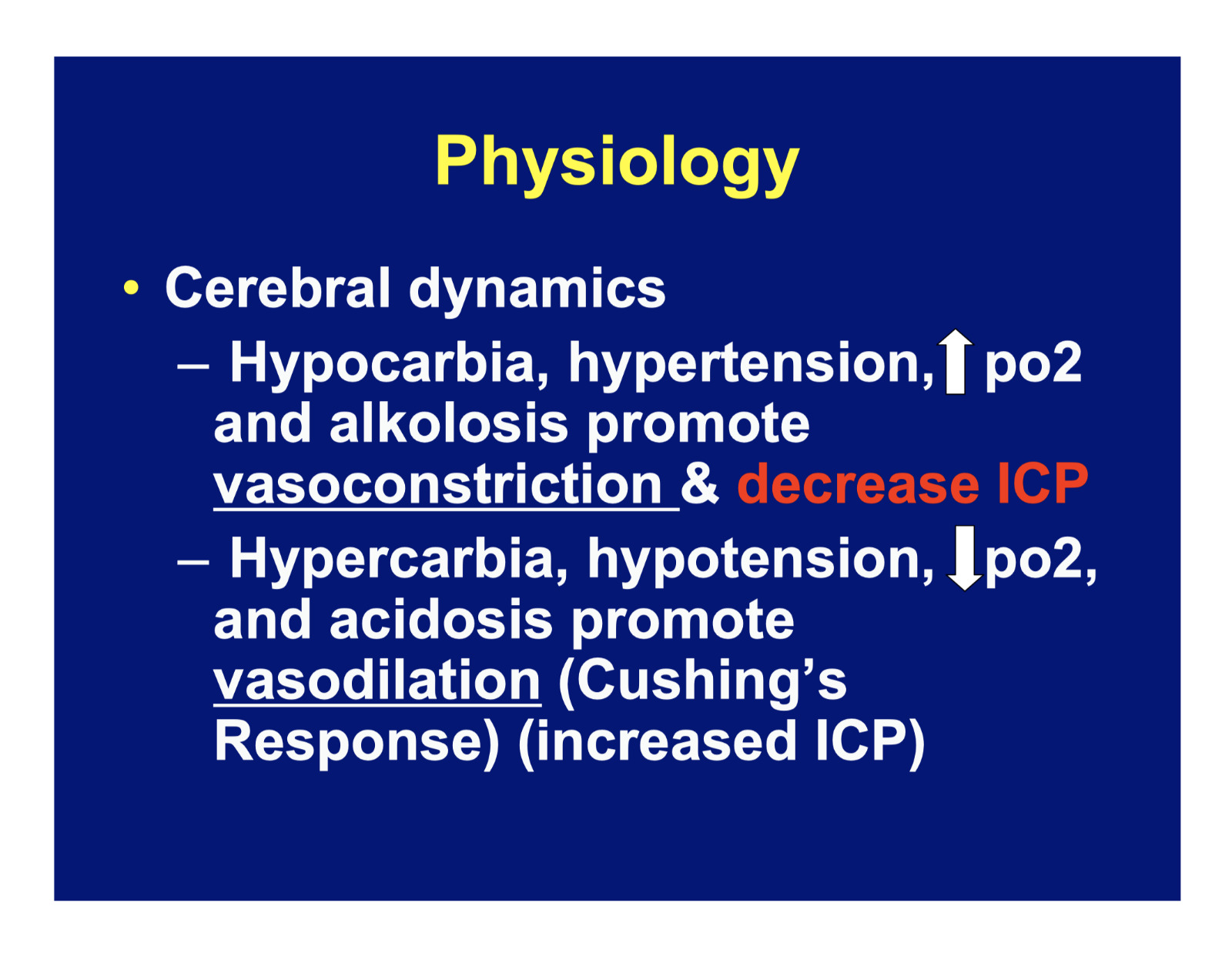
Physiology
Cerebral dynamics
Hypocarbia, hypertension, po2 and alkolosis promote vasoconstriction & decrease ICP
Hypercarbia, hypotension, po2, and acidosis promote vasodilation (Cushing’s Response) (increased ICP)Physiology
Cerebral dynamics
CBF relies upon Cerebral Profusion Pressure (CPP)
CPP = MAP – ICP
Autoregulation is lost if CPP is < 40mm Hg (normal 50-180)
Injury Patterns
Primary Injury Secondary Injury
Treatment goals must be directed at preventing hypotension, preventing hypoxia and decreasing ICP
Management
History
MOI, AMPLE, LOC
an altered level of consciousness is the hallmark of a head injury (LOC is not required)Management
Elevate patient’s head to 30 degrees
Maintain Cerebral Blood Flow (CBF)
● IV Access to treat hypotension
● Use hypertonic saline 3% in 2/ 250cc boluses reassess then maintenance fluids
● Can use NS, LR, or Hextend
Management
ABC’s
Field intubation has been shown to have a positive effect on outcome!
Get neuro exam first!
Prevent hypoxia! Maintain SaO2 > 90%Management
● Cardiac monitor if available
Know where to send head trauma
Most patients will require a CT scan and some may require a neurosurgeon
Management
● Neurological assessment
Glascow Coma Scale (q 5 minutes)
Pupillary Exam
Motor Exam
Brain Stem Function
Deep Tendon/ Pathologic reflexes
Pupillary Response
Assess pupil size and responsiveness
Large fixed pupil suggests herniation from ipsilateral lesion
NOTE: patients exposed to chemical agents or explosive blast may experience iridoplegia, which is not indicative of herniation
Motor Exam
Muscle strength
Hemiparesis contralateral to lesion
Brain Stem Function
Comatose patients
Oculocephalic response (Dolls eyes)
Oculovestibular Response (calorics)
CN III - pupillary response
CN X - Gag reflex
CN V/VII – corneal reflex
CN VII – facial longer recommended for prophylaxis. Use only for brief periods in patients showing signs of herniation
Paco2 of 30-35 mm Hg
Onset within 30 sec and peak in 8 min
Management
There is
NO
indication
for
prophylactic
hyperventilationEucapnia is good!
Management
Osmotic Diuretics
Mannitol 0.25 – 1g/kg
Effect occurs within minutes, peaks in 60 minutes and can last up to 8 hours
Reserve for neurosurgeon if possibleManagement
Steroids – No longer recommended
Broad spectrum antibiotics-
Recommend Cefoxitin
The blood brain barrier can be disrupted for many hours after trauma
Management
Seizures- 9% of blunt, 42% penetrating injury
Active seizures – Lorazepam 1-2 mg (0.05 – 0.15 mg/kg) or Diazepam 0.1mg/kg up to 5mg
Prophylaxis – Phenytoin / fosphenytoin 20mg/kg
Seizure Prophylaxis (Required)
Depressed skull fracture
Paralyzed and intubated
Seizure history
Penetrating brain injury
Severe head injury (GCS 8 or <)
Acute subdural/epidural hematoma
Acute intracranial hemorrhage
Classification and triage of TBI
Severe – GCS of 8 or < in first 48hrs (immediate evacuation)Moderate – GCS of 9 to 13 (evacuation can be delayed)Mild – GCS of 14 to 15
(observation and reassessment necessary)
Courtesy BTF guidelines
Severe Head Injury
10% of TBI who reach ED alive
Up to 25% will require surgery
Mortality 40%
Only 7% have moderate disability or good outcome.
All require CT, neurosurgey consultation and transfer to intensive neurosurgical facility
Moderate Head Injury
10% of all head injury patients
40% abnormal CT
8% lapse into coma (beware of PT that talks and deteriorates)
70% unable to work at 3mo
50% permanent disability
90% persistent HA and memory deficit
All require CT scan and ICU observation at a minimum
Minor Head Trauma/ mTBI
80% of all head injury patients
3% with mTBI will deteriorate
All patients do not require a non-contrast head CT but much controversy exists as to who does require a CTHigh Risk per Brain Injury Center
Anyone exposed to or involved in a blast, fall, vehicle crash or direct impact who becomes dazed, confused, LOC should be further evaluated for brain injury
High Risk per Brain Injury Center Signs and Symptoms
Anyone exposed to blast or MVA which causes temporally related onset of symptoms such problems
Fatigue
Insomnia/sleep disturbancesHigh Risk per Brain Injury Center Signs and remembering/concentrating
Post-Concussive Syndrome – for physical and mental
Visual Disturbances
Sensitivity to Noise
and Light
Sleep DisordersMACE Questionnaire
Screening tool for mTBI
History, neurological exam, and evaulation component
Easily administered in 5 minutes
MACE Questionnaire
Evaulation tests 4 cognitive domains
Orientation
Immediate memory
Concentration
Delayed recall
MACE Questionnaire
Scoring Significance
Non-concussed individuals have a mean total score of 28/30
A score less than 30 does not imply that a concussion has occurred
However, in the absence of baseline testing, a score of 25 or below has shown the best sensitivity and specificity for true cognitive impairment resulting from concussion
Treatment of mTBI in Theater
Four different areas:
Symptom management
Rest/return to duty guidance
Educational initiatives
Supportive therapies
Treatment of mTBI in Theater Symptom Management
Headache – acetaminophen
Avoid tramadol, narcotics, NSAIDs, ASA, or other platelet inhibitors until negative CT study
Patient educational sheet for all positive patients – provides reassurance
Bedrest – short term gain only
Profile – no exposure to possible head trauma, wearing helmet, lifting > 10lbs, running or PT, riding in military vehicles
May need SSRIs, TCAs for sleepTreatment of mTBI in Theater Rest/return to Duty
Treatment of mTBI in Theater Rest/return to Duty
Treatment of mTBI in Theater Rest/return to Duty
Treatment of mTBI in Theater
Do not return a mTBI pt to duty until fully asymptomatic
Asymptomatic pts should be exertionally tested before RTD for at least 5 minutes
Mission Impact
Unit Readiness
slowed reaction time change (100msec)
soldiers may be unable to will away symptoms
behavioral issues may ensue
Individual Issues
feel “broken”
shell shock as repeat blast mTBI exposure
irritability/ issues with family and others
associated stress reactions
mTBI Continued
Comprehensive cognitive testing performed at Level III
Implementation of baseline neurocognitive testing for high risk units (EOD, SOF, ABN)
Futher guidance on exertional testing pending
Pearls In TBI Management
Early airway management
Intubate GCS < 8Optimize oxygenationEucarbia (Do Not Hyperventilate)Volume resuscitation to euvolemia
Isotonic fluid● Normothermia
● Correct anemia
Summary
Discussed clinical spectrum of TBI
Discussed acute tx of moderate/severe TBI
Discussed assessment of mTBI pt
Introduced MACE guidelines/algorithms
Helpful Information
Specific Injuries
Epidural Hematoma
Subdural hematoma
Traumatic subarachnoid hemorrhage
Penetrating head injuries
Epidural Hematoma
Classic presentation is an altered LOC followed by a lucid interval.
Common c/o sleepiness, headache, dizziness, N/V
Subdural Hematoma
More common than EDH
Progress slowly
Decreased LOC
50-70% have lucid interval followed by decline
Unequal pupils, motor deficitTraumatic Subarachnoid Hemorrhage
Most common CT scan abnormality after head trauma
1/3 detected on first CT scan
Headache and photophobia are common complaints
Penetrating Head Injuries
76% of GSW to head die at the scene
GCS <5 associated with a near 100% mortality
GCS > than 8 has 75% survival
Basilar Skull Fracture
Blood in ear canal sign
Cranial nerve and treat hypoxia
Prevent and treat hypotension
Non-contrast head CT
Early neurological consultation
Screen for mTBI
Questions
Related Items:
SUPERMAN'S GIRLFRIEND LOIS LANE #86 WEDDING ISSUE 80 PAGE GIANT 1968
$9.99
1,035 page 68W10 / TCCC Combat Casualty Care Fieldcraft Student Handouts on CD
$14.99
Gene Autry Comics #4 CGC 8.0 Jan 1943 a 68 page classic & FREE color photocopy
$357.00