
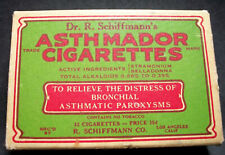
One month of tough breathing may help asthma sufferers breathe easier in the long run, according to Richard Bond, an associate professor of pharmacology at the University of Houston. Bond is challenging one of the most basic tenets of the Hippocratic Oath – first do no harm – by implementing a long-standing medical taboo to treat asthma. Although counterintuitive, Bond’s studies are reminiscent of hair-of-the-dog folk wisdom to treat like with like, in this case using beta blockers (or antagonists) instead of stimulants (or agonists) in asthmatics.
Coining the term “paradoxical pharmacology” – treating patients with medicine that initially worsens their symptoms before eventually improving their overall health – Bond first applied this hypothesis in studies with mice and then moved on to two clinical trials with humans.
Using beta blockers when it seems a stimulant is called for defies medical dogma, but this is not a new concept. Bond’s work builds on an earlier breakthrough in treating congestive heart failure (CHF). About a decade ago, the thinking on beta-blocker therapy was reversed when researchers discovered that although treatment with beta blockers reduced cardiac activity at first, the prognosis reversed itself after two to three months. This treatment shift reduced the mortality rate among CHF patients by up to 65 percent.
“Decades of conventional wisdom were overturned, and beta blockers replaced stimulants as the top drug for CHF patients,” Bond said. “For 30 years, intellect told us that beta blockers wouldn’t work to treat these patients, and unfortunately millions of heart patients died prematurely. It would be a tragedy to not have learned from that lesson.” Bond points out that beta blockers are not the only example of paradoxical pharmacology. Hyperactive children are treated with the amphetamine-like Ritalin, and the skin irritant retinoic acid is used to treat acne.
In Bond’s first clinical trial, he and his colleagues saw similar results in humans to what was seen in the mouse models. Mild asthmatics were treated for nine weeks with the beta blocker nadolol, with all subjects tolerating the drug and 80 percent experiencing a reduction in airway hyperresponsiveness. Laying the groundwork for continuing studies with beta blockers in the treatment of asthma, the results suggest there may be a way to counteract some of the negative aspects of traditional treatments.
“The principle that certain pharmacological compounds have different effects depending upon whether they are given for long or short periods has been demonstrated,” Bond said. “And even if I am correct about beta blockers ultimately being used in the treatment of asthma, there probably always will be a need for the inhaler-type agonist drugs to handle acute asthma attacks. I do believe, though, that beta blockers hold promise in a maintenance or preventative regimen that could reduce the number or severity of attacks and improve a patient’s quality of life.”
Related:
Asthma Could Be Several Distinct Diseases
Pool Chlorine Implicated In Childhood Asthma
Prof Pooh-Poohs Western World’s Anti-Bacterial Crusade












Comments are closed.