
With the H5N1 bird flu virus now spreading into Western Europe, governments are at last seriously focusing on what can be done to avert a pandemic if it mutates into a strain that can be passed from human to human. Behind the scenes, scientists are scrambling for answers in the knowledge that current anti-viral stockpiles may not be affective. This has prompted one group of British chemists to urge that a DNA vaccine be considered.
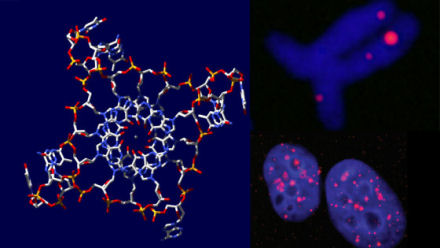
DNA vaccines are cutting edge anti-viral technology that have to date, had only very limited trials in humans. Despite the lack of trials to demonstrate their safety and effectiveness, vaccines based on DNA could be a viable option, say British biochemical engineers, writing in the journal Biotechnology Progress. DNA vaccines, they say, can be produced more rapidly than conventional vaccines and might save thousands of lives if a global influenza outbreak does occur.
If the virus did mutate to allow human-to-human transmission, then traditional vaccine production facilities are unlikely to be able to meet global demand in time to avert a pandemic, says chemist Peter Dunnill at University College London. But, he added, it might be possible to quickly produce a DNA vaccine by adapting the manufacturing processes of selected pharmaceutical and antibiotic plants.
Dunnill stressed that if a DNA vaccine were going to be used, decisions would have to be made now. “If we’re going to try it, we need to move. You can’t expect to walk into a production facility, hand over the instructions, and expect them to make it on the spot. It’s going to take some weeks, and we really don’t know how much time we have.” Dunnill believes that a DNA vaccine could be produced in as little as two or three weeks, in contrast to conventional vaccines, which can take up to six months.
The technique is largely untested in humans, although it has worked well in animals, and Dunnill believes that human trials could be accelerated, particularly if the H5N1 virus eventually causes large numbers of deaths and outpaces the supply of conventional vaccine. In the worst case scenario, he concludes, using a DNA vaccine could be a “stop-gap” measure until enough conventional vaccine is available.







Comments are closed.